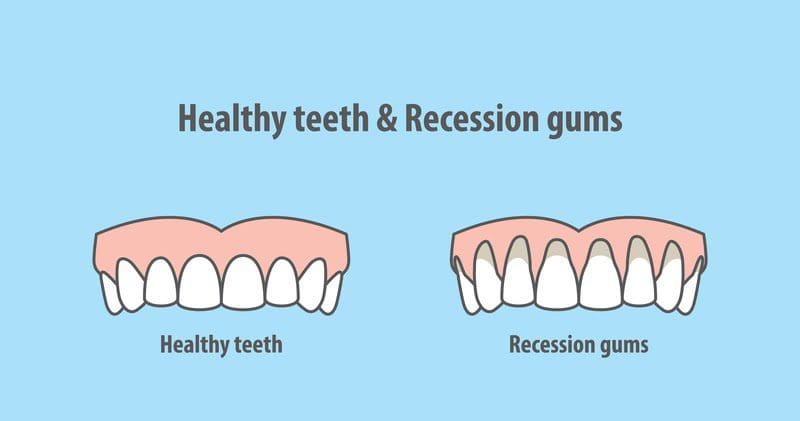
Gum recession and its symptoms: Gum recession occurs when the height of the gum tissue around the teeth recedes and migrates downward toward your jaw bone, making your teeth appear longer than normal. The root portion of the tooth is exposed, which can cause the tooth to be more sensitive to cold, sugary, or acidic foods. You may see a yellow zone underneath the tooth itself due to the color difference between enamel and cementum (surface covering of the root). Gum recession results in “pockets” between the teeth and the gum line, causing the entrapment and build-up of food residue and bacteria. Gum recession typically occurs over a span of many years. Contrary to common belief, gum recession is not a disease of aging. Unlike bone, gum tissue doesn’t grow back, so early detection and prevention is critical. Below are some common causes for gum recession and recommended prevention methods.
Gum disease is by far the most common cause for sudden or aggressive gum recession. Gum disease occurs when the gum surrounding the tooth becomes inflamed due to plaque (biofilm) formation. 80% of the population has some form of gum disease (aka gingivitis — red, puffy and swollen gums; gums bleeding while brushing or flossing; bad breath; etc.) while 50% have a severe form of gum disease (periodontitis). If left untreated, periodontitis can lead to bone loss and tooth loss. Furthermore, the bacteria responsible for periodontitis can enter the bloodstream and increase the risk of heart attacks, diabetes, rheumatoid arthritis, respiratory disease, and Alzheimer’s disease. Gum disease is largely preventable through daily brushing, flossing and regular dental cleanings. During the routine dental cleaning appointment, your hygienist will assess the health of your gum tissue through periodontal charting. Pay attention to any “hot spots”. Milder cases of gum disease can be treated by professional dental cleanings (scaling and root planing) to remove tartar (calculus) build up. Severe cases of gum recession as a result of advanced periodontitis may require dental surgery such as gingival grafting or flap surgery.
Aggressive brushing and/or flossing: Using excessive force, a horizontal brushing motion, or an old, worn nylon brush that has lost its end-rounding or polish can cause damage to the gum line. Change your toothbrush often, and use a circular motion when brushing. Discuss proper brushing techniques with your hygienist during your next cleaning appointment.
Aggressive orthodontics: Brackets, wires, bands, etc. that glue to the tooth can lead to plaque buildup and inflammation of the gums. The very thin edge of the gums may necrotize (die off). Discuss with your dentist to see if you are a good candidate for Invisalign, since the aligner trays are removable for brushing and flossing.
Food trauma: Foods like coarse cereal, pork rinds, hard bread crust, and thick tortilla chips can scrape the gums. The hull of popcorn can get caught between the gum and the tooth and cause inflammation. Chew slowly and eat small bite-sized pieces. If your gums become irritated by food, be proactive and schedule a visit with your dentist as soon as possible.
Grinding and clenching due to stress and sleep apnea can put a lot of vertical force on the gums and bone, resulting in gum recession.
Crowding of the teeth, particularly at the lower anterior when one tooth is staggered and the tooth next to it is pushed back. This creates a three-walled pocket where food can get caught and cause inflammation. Consider orthodontic adjustments to address crowding.